[ad_1]

Context:
There is considerable excitement in the world of medicine after scientists reported that a woman living with HIV (Human Immunodeficiency Virus) and administered an experimental treatment is likely ‘cured’. Only three people so far are known to have been cured of HIV.
A patient with leukaemia in the United States has become the first woman and the third person to date to be cured of HIV after receiving a stem cell transplant, researchers say.
What is HIV and how is it transmitted?
Human immunodeficiency virus or HIV is an infection that attacks the immune system by destroying the body’s immune cells called CD4, which help it respond to infection.
Once HIV attacks the CD4 cells, it starts replicating and destroying the cells, weakening the body’s immune system and making it more prone to certain “opportunistic infections” that take advantage of the weak immune system.
Bodily fluids such as blood, semen, vaginal fluids, rectal fluids and breastmilk can be carriers for HIV.
It can be transmitted through unprotected sex, transfusion of contaminated blood, sharing needles and syringes, and from a mother with HIV to her infant during pregnancy.
Typically, the time between HIV transmission and AIDS diagnosis is 10-15 years, although it may occur sooner.
What do we know about the treatment?
- At Conference on Retroviruses and Opportunistic Infections, Colorado, United States, Researchers described the case of a 60-year-old African American woman who was diagnosed with an HIV infection in 2013 was started on the standard HIV treatment regimen of anti-retroviral treatment (ART) therapy consisting of tenofovir, emtricitabine and raltegravir. She was also later diagnosed with leukemia in 2017.
- In that year she received cord blood, or embryonic stem cells, from a donor with a rare mutation that naturally blocks the HIV virus from infecting cells. She was also given blood stem cells, or adult stem cells, from a relative.
- The adult stem cells boosted the patient’s immunity and possibly helped the cord blood cells fully integrate with the lady’s immune system.
- A little over three years after the transplant, the lady discontinued the ART and today more than 14 months down, her doctors report that she has no sign of HIV in her blood and also has no detectable antibodies to the virus.
- Embryonic stem cells are potentially able to grow into any kind of cell and hence their appeal as therapy, though there is no explanation for why this mode of treatment appeared to be more effective.
What is unique about the recovery of this woman?
Only two people have reportedly been cured of HIV so far and both have relied on bone marrow transplants from donors who carried the mutation, called CCR5 delta 32, that naturally makes one immune to an HIV infection and AIDS.
However, the previous transplants involved adult stem cells and these cells from the bone marrow replaced their immune system.
The body’s natural tendency is to reject foreign stem cells and so both donors suffered side effects such as graft versus host disease where the donor’s cells attack the recipient’s body.
Both men developed severe illnesses throughout their HIV remission but in contrast the woman was discharged from hospital within 17 days of the transplant and did not develop graft versus host disease.
Her doctors theorise that it was a combination of the embryonic and adult stem cells that led to a better health outcome.
However, because it’s only been five-odd years of being HIV-free, it remains to be seen if the lady will live longer than Brown or Castillejo.
How umbilical cord blood was used to cure an HIV patient?
The woman’s treatment involved umbilical cord blood, unlike the two previous known cases where patients had received adult stem cells as part of bone marrow transplants.
Umbilical cord blood is more widely available than the adult stem cells previously used and it does not require as close a match between donor and recipient.
President-elect of the International Aids Society, cautioned that the transplant method used in this case wouldn’t be a viable cure for most people living with HIV.
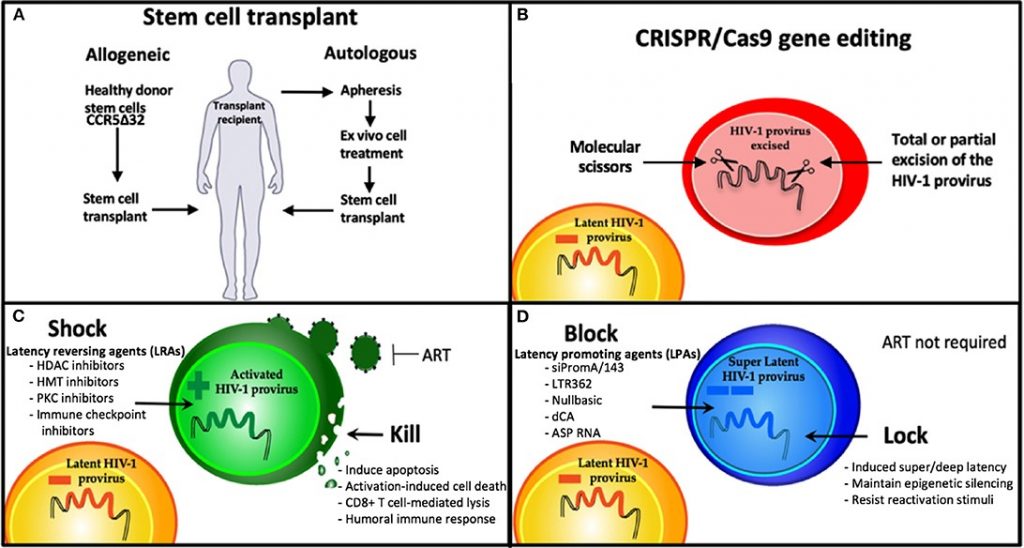
But she added that the case “confirms that a cure for HIV is possible and further strengthens using gene therapy as a viable strategy for an HIV cure.”
The findings around this most recent case study are yet to be published in a peer-reviewed journal, so wider scientific understanding is still limited.
What is the prevalence of HIV/AIDS in India?
As per the India HIV Estimation 2019 report, the estimated adult (15 to 49 years) HIV prevalence trend has been declining in India since the epidemic’s peak in the year 2000 and has been stabilising in recent years.
In 2019, HIV prevalence among adult males (15–49 years) was estimated at 0.24% and among adult females at 0.20% of the population.
There were 23.48 lakh Indians living with HIV in 2019. Maharashtra had the maximum at 3.96 lakh followed by Andhra Pradesh (3.14 lakh) and Karnataka.
India’s National Aids Control Organisation says that ART is “freely available” to all those who require and there are deputed centres across the country where they can be availed from.
Conclusion: Is this treatment the long-sought cure for AIDS?
Not at all. While this approach is certainly a welcome addition to the arsenal of treatments, stem cell therapy is a cumbersome exercise and barely accessible to most HIV patients in the world.
Moreover, this requires stem cells from that rare group of individuals with the beneficial mutation.
Anti-retroviral therapy, through the years, has now ensured that HIV/AIDS isn’t always a death sentence and many with access to proper treatment have lifespans comparable to those without HIV.
A vaccine for HIV or a drug that eliminates the virus is still elusive and would be the long sought ‘cure’ for HIV/AIDS.
[ad_2]